Section 3 | Tackling Clinical Mastitis
Page 14 /
Gram Positive Bacteria
The caveat must again be raised: you should discuss and develop all treatment protocols with your herd veterinarian.
The information presented here is for your learning purposes and should not constitute medical advice
That being said, there are some important pathogen-specific characteristics to know about the culture results you receive.
Staphylococcus aureus (a.k.a. Staph. aureus)
Staph. aureus is a pretty big deal as a culture result. Staph. aureus is a contagious bacteria. It can live in and on the cow and is often passed from cow to cow at milking time. It can also be present in the environment. Flies can play a role in the infection of cows and heifers. It is notoriously difficult to treat with antimicrobials. The bacteria has a variety of survival tactics that make it difficult to cure:
- It can form microabscesses in the udder. These microabscesses are sheltered from the cow’s white blood cells. Also, antimicrobials cannot reach them there
- Different strains of Staph. aureus have lower sensitivity to antimicrobial treatments
- They have a lot of weapons. Some attack the cow’s cells. Others camouflage the bacteria to evade the cow’s defenses

Source: ACER Consulting Ltd.
These factors create a difficult situation for the cow. Treatment attempts are often unsuccessful. Cure rate estimates range between 4-90%1, so it’s important to understand the factors that drive treatment success and failure.
An excellent review article has been produced that can help you and your veterinarian determine the best course of action when confronted with Staph. aureus mastitis1. The probability of a cure is LOWER:
- In older cows
- Heifers have the best chances for treatment success
- As somatic cell count (SCC) increases
- The higher the SCC, the lower the chances of treatment success
- If the infection has been there for a long period
- The longer the infection, the lower the likelihood of treatment success
- As more quarters are affected
- In hind quarters
Keep these points in mind when you’re designing treatment protocols with your herd veterinarian.
If you have decided that the infected cow has a relatively good chance for cure (e.g. first calf heifer recently infected in a front quarter with an SCC of 250,000 cells/mL), there is evidence that supports using extended antimicrobial therapy with an approved product in these animals2. Again, your veterinarian will be able to guide you in the appropriate course of action, should you deem treatment warranted.

Coagulase Negative Staphylococcus (CNS)
These bacteria are seen as minor pathogens. They live on and around the cow. They don’t have as many weapons and defenses as Staph. aureus does. As such, they are far more easily treated. The use of any lactating cow intramammary antimicrobial at label dose and duration should give you a good chance at curing infections2.
Streptococcus
These groups of bacteria predominantly live in the cow’s environment. Infections occur between milkings in the barn environment. Much like CNS, most of these species are responsive to most lactating cow intramammary antimicrobials at label dose and duration2.
A Special Exemption: Streptococcus uberis
As with most Streptococcus species, S.uberis lives in the environment of the cow. One thing that makes this species unique is that some strains are able to establish chronic (long term) infections in the udders of cows. This means that they can also look like contagious bugs, passing from cow to cow at milking time3. Because of this, some research supports the on-label use of intramammary antimicrobial treatments for extended periods (5-8 days) when treating S.uberis4, 5.
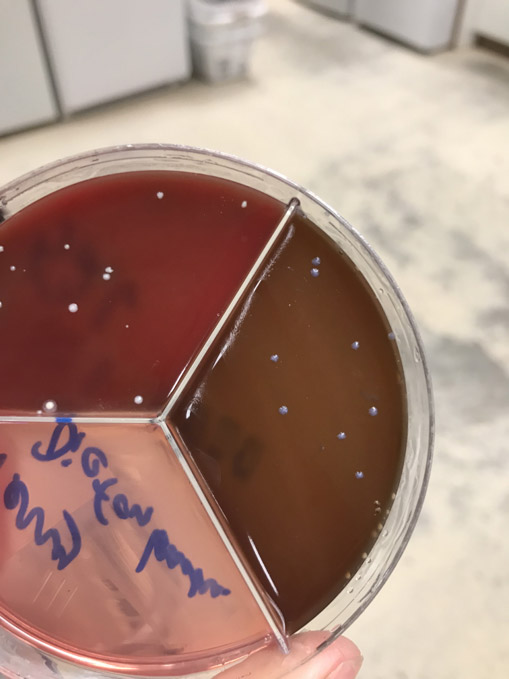
Source: ACER Consulting Ltd.
References
- Barkema H.W., Schukken Y.H., Zadoks R.N. Invited Review: The role of cow, pathogen, and treatment regimen in the therapeutic success of bovine Staphylococcus aureus mastitis. J. Dairy Sci. 2006/05/17. 2006;89(6):1877-95.
- Royster E., Wagner S. Treatment of Mastitis in Cattle. Vet. Clin. North Am. Food Anim. Pract. 2015;31(1):17-46.
- Davies P.L., Leigh J.A, Bradley A.J, Archer S.C, Emes R.D, Green M.J. Molecular epidemiology of Streptococcus uberis clinical mastitis in dairy herds: Strain heterogeneity and transmission. J. Clin. Microbiol. 2016;54(1):68-74.
- Truchetti G., Bouchard E., DesCoteaux L., Scholl D., Roy J.P. Efficacy of extended intramammary ceftiofur therapy against mild to moderate clinical mastitis in Holstein dairy cows: A randomized clinical trial. Can. J. Vet. Res. Can. Rech. Vet. 2014;78(1):31-7.
- Gillespie B., Moorehead H., Lunn P., Dowlen H., Johnson D., Lamar K., et al. Efficacy of extended pirlimycin hydrochloride therapy for treatment of environmental Streptococcus spp and Staphylococcus aureus intramammary infections in lactating dairy cows. Vet. Ther. 2002;3(4):373-80.